The preparedness and adaptability of our public health infrastructure is critical in the event of a biological incident (i.e., bioterrorism) [1, 2]. Unfortunately, many health care facilities and administrators have acquired a sense of complacency and are inadequately prepared to deal with the reality of bioterrorism [3, 4].
To address these concerns, this article covers important considerations for hospitals and health care workers in the wake of a biological incident. These considerations are divided into three distinct phases: pre-incident preparedness, preservation of life and resources during an incident, and post-incident response.
Phase 1: Pre-Incident Preparedness
There is a possibility that the U.S. may encounter a threat pathogen (either natural or intentional) in the near future [5]. The number of fatalities during a biological incident depends not only on the nature and location of the threat, but also the ability to react and effectively treat the wounded [5].
Health care systems across the U.S. and all levels of government continuously engage in preparedness-based activities to minimize potential threats, safely treat victims, and minimize loss of life [6].
Infrastructure Preparedness: Hospital Accreditation
For health care facilities, preparedness against threats like bioterrorism begins with hospital accreditation. The largest independent non-profit health care accreditation organization in the U.S. is The Joint Commission (TJC), which accredits over 75% of hospitals and most Department of Defense health facilities [7, 8]. In order to receive federal funding, the Centers for Medicare and Medicaid require TJC accreditation.
The accreditation program requires the successful implementation of more than 50 key points to ensure compliance, some of which are pertinent to bioterrorism, including:
1) Agreement with an Outside Blood Supplier
- An outside blood supplier ensures that hospitals can sustain life among multiple casualties during both normal operations and a potential crisis
2) Infection Control Plan
- An infection control plan is essential for the day-to-day operation of any health care facility and is of critical importance during a communicable disease outbreak. Staff should be trained and adequately protected from an array of different pathogens. Patients should be properly isolated, and non-suspected patients should be protected from cross contamination.
3) Patient Flow Documentation
- This can include triage and isolation of suspected infected patients and separation from the general hospital (non-infected population).
4) Emergency Operations Plan (EOP) and Annual Evaluation
- Conduct a Hazard Vulnerability A n a l y s i s , a s p e r s t a n d a r d EM.01.01.01, EM.03.01.01, to inform development of an EOP [7].
- EOP also includes proper staffing, logistics, triage, and the full spectrum of activities during emergency operations.
5) Emergency Management Drill Records and After-Action Reports
- These drills can be “all hazard” type of incidence and are good practice to test the hospital’s incident management system in order to effectively identify recommendations for afteraction reports.
- Hospitals generally don’t conduct emergency management drills on their own, but since it is a requirement for accreditation, hospitals are better positioned to conduct emergency readiness activities [5].
Federal Preparedness
Several laws grant the U.S. Health and Human Services (HHS) secretary national authorities in response to a potential biological threat. These laws include, but are not limited to, the Pandemic and AllHazards Preparedness Act, the Public Readiness and Emergency Preparedness Act, and the Public Health Service Act [9].
If any of these emergency powers is invoked, the HHS secretary may enforce broad legal authorities to support federal, state, and local entities for declared or undeclared public health emergencies. Such actions include:
1) Implementing procedures to assist state and local governments to control epidemics and mitigate other medical emergency situations.
2) Allocating resources for research studies to better understand the etiology and medical counter measures (MCM) to treat or mitigate the spread of threat pathogens
3) Establishing isolation and quarantine centers.
4) Authorizing the Food and Drug Administration (FDA) to temporarily allow usage of a medical device or treatment if the product can further prevent loss of life and alleviate suffering (Emergency Use Authorization).
Phase 2: During a Biological Incident
Indications of a Biological Incident
The national surveillance of infectious dis-eases is paramount in controlling potential epidemics. Syndromic surveillance, or the collection of symptom and health-related data, aids in the early detection of patterns signaling a possible bioterrorism attack.
While this approach forms the backbone of the National Electronic Disease Surveillance System and the World Health Organization’s Global Outbreak Alert and Response Network, reports of non-specific illnesses weaken the specificity of such systems [10].
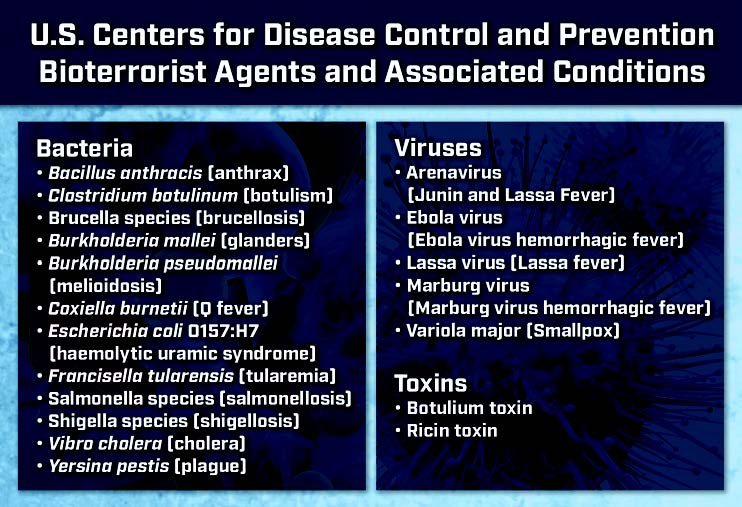
It is often frontline health care professionals in clinics, emergency departments, and pharmacies that first encounter potential biological threats as an increased number of patients seek medical care. Therefore, it is critical that health care professionals recognize the various symptomatology of viral and bacterial infections—especially since non-specific symptoms (such as fever and malaise) are typically the initial presentation. Other clinical indications of a biological incident may include a rise in unexplained illnesses, a single incident of a rare pathogen (e.g., anthrax), and atypical routes of exposure. Several potential biological threats are listed in Table 1.
Once a potential threat has been identified, confirmatory testing is the next step to initiate the appropriate cascade of medical countermeasures. In the last decade, there have been tremendous advancements in sequencing technologies to permit rapid and accurate pathogen detection. Portable systems allow health care workers to diagnose and communicate results in a matter of hours. For example, a cartridge-based assay has been developed for tularemia and anthrax, while rapid antibody assays can now diagnosis Ebola and Lassa virus [11, 12]. At the initial point of care, blood, sputum, and nasal cultures should be sent for evaluation along with a complete panel of blood work.
Protection of Health Care Personnel
The protection of health care workers is of critical importance during a biological incident. Doctors, nurses, and other medical personnel are at serious risk of exposure and may unknowingly propagate the spread of infectious agents after contact with patients.
Personal protective equipment (PPE) provides a reliable and immediate first line of defense to reduce the risk of exposure. PPE refers to clothing and respiratory devices that shield individuals from chemical, physical, or biological hazards. There are four tiers of PPE protection (A–D), with A conferring maximum protection, and D the least protection.
Most health care workers are familiar with Level D PPE (hospital gown, goggles, surgical mask, and latex gloves). Person-to-person transmission is exceedingly rare when Level D PPE guidelines are appropriately followed, and patients can be cared for without isolation units or specialized respiratory devices. However, Level D PPE is inappropriate for hemorrhagic viruses (Ebola, Marburg, Lassa, and Muchupo), smallpox virus, aerosolized pathogens, and, to a lesser extent, Y. pestis. Unless the agent can be unambiguously identified as non-life-threatening, Occupational Safety and Health Administration regulations call for Level B protection [13].
Level A protection is necessary for Ebola and requires fluid-resistant body suits, cover aprons, double gloves, shoe covers, and an air-purifying respirator [14]. These stringent guidelines were difficult to realize in Africa and led to the death of more than 300 health care workers during the Ebola outbreak of 2014 [15]. This example highlights how proper access to the appropriate level of PPE is essential to mitigate cross-contamination and preserve the lives of health care workers.
Vaccines are venerable MCMs that arguably confer the best protection against infectious diseases. Commercial vaccines are available for a wide array of viral and bacterial diseases including anthrax, smallpox, botulinum toxin, ricin, Y. pestis, tularemia, and Junin virus. No vaccines for hemorrhagic fevers have been licensed apart from yellow fever and Junin virus. However, a new vaccine for Ebola is under development that proved successful in the 2018 epidemic in the Democratic Republic of the Congo [16].
In contrast to PPE, vaccines have many pragmatic limitations that hinder their application during a biological incident. First, it is not standard practice to preemptively vaccinate health care workers or the general public against common biological agents used in warfare. According to the Centers for Disease Control and Prevention, routine smallpox vaccination stopped in 1972 after the disease was eradicated in the U.S. [17]. Second, vaccination demands knowledge of the pathogen prior to inoculation and an induction time is necessary to generate a robust antibody response. Third, some vaccines, such as the anthrax vaccine, require multiple shots and boosters on different days to confer protection.
When taken together, the urgency and uncertainty that surrounds a biological incident restricts the power of many vaccines to pre-exposure prophylaxis. These limitations are minimalized when vaccines are administered to health care workers and first responders before potential threats unfold. Of note, an effective post-exposure prophylaxis vaccine is available for smallpox when administered three or four days following exposure [18].
Table 1. U.S. Centers for Disease Control and Prevention Bioterrorist Agents and Associated Conditions
Vulnerable Populations
In the context of a public health emergency, children and the elderly constitute the largest vulnerable populations. Children have specific physiologic vulnerabilities, such as increased skin surface area and faster respiratory rate, metabolism, and cell division portending greater susceptibility to biological agents [19]. Various stages of behavioral development increases their risk for post-traumatic stress disorder (PTSD) and other acute stress disorders, while physical limitations can lead to various levels of dependency on adult care.
Both doxycycline and ciprofloxacin are relatively contraindicated in pregnant women and children under the age of twelve, and should only be administered if no other alternatives exist. With respect to the elderly, the disruption of key resources or services during an incident may have detrimental consequences to their overall health and impact their ability to respond to threats.
Phase 3: Post-Incident Response
Decontamination
Decontamination is of paramount importance in the wake of a biological incident. Most viruses and non-spore forming bacteria are sensitive to alcohols, bleach, ultraviolet light, and commercial disinfectants containing tetraalkylammonium salts. The versatility of alcohols has been somewhat compromised by their pervasive use, leading to a notable increase in resistance to ethanol and isopropanol in hospitals around the world [20].
In general, decontamination should occur as soon as possible to reduce potential exposure. Soapy water is advised for mass decontamination due to its abundant onsite availability and low potential for adverse reactions. Although diluted solutions of commercial bleach are also highly effective, bleach irritates mucous membranes and should not be used on open wounds. PPE can be sufficiently decontaminated with bleach without issues. Note that children and the elderly are more susceptible to hypothermia during decontamination and should be thermally insulated after exposure to cold water [21].
Critical Infrastructure Vulnerability Assessment
It is imperative that hospitals conduct frequent infrastructure vulnerability assessments to identify and address potential weaknesses, mitigate unnecessary human suffering, and execute proper management of limited supplies [22]. Examples of potential infrastructure vulnerabilities include:
1) Facility contamination
2) Limited communication capabilities
3) Security concerns (lack of perimeter protection, riots, etc.)
4) Lack of utilities such as clean water, electricity, and waste management
5) Lack of minimal staffing and logistics to sustain operations
Sustainment of Care and Continued Use of MCMs
Supportive treatment and assessment of airway, breathing, and circulatory systems remains the cornerstone for any biological incident given that many clinical presentations are non-specific. Rapid diagnosis of anthrax, botulism, and plague are paramount, as mortality can be prevented with timely administration of antibiotics, antisera, and/or vaccines. Working off a presumptive diagnosis and initiating prompt treatment is crucial as the prodrome phase of many biological agents is when treatment is most effective (Y. pestis is universally fatal if treatment is delayed by more than a day). At the time of this writing, doxycycline is generally effective against B. anthraces, Y. pestis, Brucella, Coxiella, and F. tularensis.
For certain viral infections, nucleoside analogues are highly effective MCMs that should be generously distributed post incident. Cidofovir was found to be more effective at preventing mortality in non-human primates infected with monkeypox virus than post-exposure vaccines—suggesting that antivirals may play an important role in mitigating a potential smallpox outbreak [23]. Although the FDA has yet to approve any antiviral agents for hemorrhagic viruses, GS-5734 is currently in clinical trials for the treatment of persistent Ebola virus [24].
The continued use of appropriate MCMs, such as vaccines, antivirals, and antibacterial agents, should be widely implemented for several days after an incident to prevent future manifestations of disease. Note that quarantine can be problematic for those with a suspected exposure, since the population would consist of both exposed and unexposed, thus potentially driving transmission [25].
Individuals that remain unexposed still have the potential to suffer from unrelated physical and behavioral ailments and health care providers must be prepared to address their psychological needs. A robust and proactive line of communication from public health and other government authorities is crucial to allay concerns and help mitigate mass panic. Such a traumatic event has the potential to trigger PTSD in survivors and unexposed alike, and access to behavioral health experts in the aftermath is important to debrief and process the event.
Conclusion
Hospitals and healthcare workers play a pivotal role in ensuring that preparedness protocols are properly followed and executed during a biological incident to reduce suffering, mitigate exposure, and preserve human life.
While the incidence rate of bioterrorism on U.S. soil is relatively low, preparedness exercises should be practiced regularly to swiftly counter a potential threat. Recent trends toward highly coordinated terrorist tactics significantly increase health care vulnerability to covert attacks and bolsters the need to ensure a top-notch preparedness program. This is a shared responsibility among healthcare administrators, communities, and all levels of government to promote homeland defense and preservation across the healthcare spectrum.
References
- Grundmann, O. (2014). The current state of bioterrorist attack surveillance and preparedness in the US. Risk Management and Healthcare Policy, 7, 177-187. doi:10.2147/ RMHP.S56047
- Bennett, R. L. (2006). Chemical or biological terrorist attacks: an analysis of the preparedness of hospitals for managing victims affected by chemical or biological weapons of mass destruction. International Journal of Environmental Research and Public Health, 3(1), 67-75.
- Finucane, D. J. (2018). Unhealthy complacency: The vulnerability of US hospitals to direct terrorist attacks. Journal of Healthcare Risk Management, 37(3), 8-12. doi:10.1002/ jhrm.21282
- Jacobs-Wingo, J. L., Schlegelmilch, J., Berliner, M., Airall-Simon, G., & Lang, W. (2019). Emergency preparedness training for hospital nursing staff, New York City, 2012-2016. Journal of Nursing Scholarship, 51(1), 81-87. doi:10.1111/jnu.12425
- Toner, E. (2017). Healthcare preparedness: Saving lives. Health Security, 15(1), 8-11. doi:10.1089/hs.2016.0090
- U.S. Department of Health and Human Services (2014). 2014 public health emergency medical countermeasures enterprise (PHEMCE) strategy and implementation plan. Retrieved from https://www.phe. gov/Preparedness/mcm/phemce/Documents/2014-phemce-sip.pdf.
- The Joint Commission. (2017). Accreditation Guide for Hospitals. Retrieved from https://www.jointcommission.org/assets/1/18/171110_Accreditation_Guide_ Hospitals_FINAL.pdf
- U.S. Department of the Navy. (2008). DoD information assurance certification and accreditation process (DICAP) handbook. Retrieved from http://acqnotes.com/acqnote/careerfields/dod-information-assurance-certification-and-accreditation-process-diacap
- U.S. Department of Health & Human Services. (2018). Legal authority of the secretary. Retrieved from https://www.phe.gov/ Preparedness/support/secauthority/Pages/default.aspx
- Kaufman, Z., Wong, W. K., Peled-Leviatan, T., Cohen, E., Lavy, C., Aharonowitz, G., . . . Green, M. S. (2007). Evaluation of a syndromic surveillance system using the WSARE algorithm for early detection of an unusual, localized summer outbreak of influenza B: Implications for bioterrorism surveillance. Israel Medical Association Journal, 9(1), 3-7.
- Banada, P. P., Deshpande, S., Chakravorty, S., Russo, R., Occi, J., Meister, G., . . . Alland, D. (2017). Sensitive detection of francisella tularensis directly from whole blood by use of the GeneXpert system. Journal of Clinical Microbiology, 55(1), 291-301. doi:10.1128/jcm.01126-16
- Satterly, N. G., Voorhees, M. A., Ames, A. D., & Schoepp, R. J. (2017). Comparison of MagPix assays and enzyme-linked immunosorbent assay for detection of hemorrhagic fever viruses. Journal of Clinical Microbiology, 55(1), 68-78. doi:10.1128/jcm.01693-16
- U.S. Department of Labor. (2005). OSHA/ NIOSH interim guidance. Retrieved from https://www.osha.gov/SLTC/emergencypreparedness/cbrnmatrix/chemwarfare.html
- Stephens, D. S., Ribner, B. S., Gartland, B. D., Feistritzer, N. R., Farley, M. M., Larsen, C. P., & Fox, J. T. (2015). Ebola virus disease: Experience and decision making for the first patients outside of Africa. PLoS Medicine, 12(7), e1001857. doi:10.1371/ journal.pmed.1001857
- Green, A. (2014). Remembering health workers who died from Ebola in 2014. The Lancet, 384(9961), 2201-2206.
- Green, M. S., LeDuc, J., Cohen, D., & Franz, D. R. (2019). Confronting the threat of bioterrorism: Realities, challenges, and defensive strategies. The Lancet Infectious Diseases, 19(1), e2-e13. doi:https://doi. org/10.1016/S1473-3099(18)30298-6
- Centers for Disease Control and Prevention. (2017). Vaccine basics. Retrieved from https://www.cdc.gov/smallpox/vaccine-basics/index.html
- Henderson, D. A., Inglesby, T. V., Jr., O’Toole, T., & Mortimer, P. P. (2003). Can postexposure vaccination against smallpox succeed? Clinical Infectious Diseases, 36(5), 622-629. doi:10.1086/374054
- Bartenfeld, M. T., Peacock, G., & Griese, S. E. (2014). Public health emergency planning for children in chemical, biological, radiological, and nuclear (CBRN) disasters. Biosecur Bioterror, 12(4), 201-207. doi:10.1089/ bsp.2014.0036
- Pidot, S. J., Gao, W., Buultjens, A. H., Monk, I. R., Guerillot, R., Carter, G. P., . . . Stinear, T. P. (2018). Increasing tolerance of hospital Enterococcus faecium to handwash alcohols. Science Translational Medicine, 10(452). doi:10.1126/scitranslmed.aar6115
- U.S. Department of Homeland Security (2014). Patient decontamination in a mass chemical exposure incident: National planning guidance for communities. Retrieved from https://www.dhs.gov/sites/default/files/ publications/Patient%20Decon%20National%20Planning%20Guidance_Final_December%202014.pdf
- Banach, D. B., Johnston, B. L., Al-Zubeidi, D., Bartlett, A. H., Bleasdale, S. C., Deloney, V. M., . . . Trivedi, K. K. (2017). Outbreak response and incident management: SHEA guidance and resources for healthcare epidemiologists in United States acute-care hospitals. Infection Control and Hospital Epidemiology, 38(12), 1393-1419. doi:10.1017/ ice.2017.212
- Israely, T., Paran, N., Lustig, S., Erez, N., Politi, B., Shafferman, A., & Melamed, S. (2012). A single Cidofovir treatment rescues animals at progressive stages of lethal orthopoxvirus disease. Virology Journal, 9, 119-119. doi:10.1186/1743-422X-9-119
- Warren, T. K., Jordan, R., Lo, M. K., Ray, A. S., Mackman, R. L., Soloveva, V., . . . Bavari, S. (2016). Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in Rhesus monkeys. Nature, 531, 381. doi:10.1038/nature17180
- Barbera, J., Macintyre, A., Gostin, L., Inglesby, T., O’Toole, T., DeAtley, C., . . . Layton, M. (2001). Large-scale quarantine following biological terrorism in the United States: Scientific examination, logistic and legal limits, and possible consequences. JAMA, 286(21), 2711-2717.


