In his seminal work, “Democracy in America,” Alexis de Tocqueville warned against “the tyranny of the majority” – the idea that decisions would be made by a majority who placed their interests above those of individuals or minority groups. While this term usually refers to political decisions, the principle can be applied to a number of scenarios in which a ruling group makes decisions that must be followed by the non-majority. These types of decisions often occur in medicine as a physician typically recommends a course of treatment based on his training and the published advice of experts. The modern practice of medicine is keenly focused on administering treatment based on scientific evidence. While heralded as the gold standard, scientific practice often overlooks other important deciding factors in a patient’s care, such as religion, ethnicity and cultural knowledge. The debate on vaccination is a signature example of the conflict between science
and belief, and another emerging debate could involve the use of nanotechnology in medical applications, often termed nanomedicine.
Nanotechnology is the manipulation of matter on an atomic scale, typically the creation and use of materials between one and 100 nanometers. These materials are referred to as engineered nanomaterials. The concept was first introduced in 1959 by the famed physicist and Nobel Laureate Richard Feynman during a lecture he gave at the California Institute of Technology titled “There’s Plenty of Room at the Bottom.” Although the word nanotechnology was never used, his speech laid the groundwork for what would become another technological revolution. In this speech, Feynman declared, “It would be interesting in surgery if you could swallow the surgeon. You put the mechanical surgeon inside the blood vessel, and it goes into the heart and ‘looks’ around. It finds out which valve is the faulty one and takes a little knife and slices it out. Other small machines might be permanently incorporated in the body to assist some inadequately-functioning organ.” [1]
Medical applications of nanotechnology span a range of possibilities, but they generally fall into four categories:
• Diagnostics and imaging;
• Pharmaceutical and drug-delivery systems;
• Regenerative medicine/tissue engineering/surgery; and
• Implantable devices
![Figure 1: Comparison of nanoscale materials with common objects. [16] (Released)](https://hdiac.org/wp-content/uploads/2015/07/201506-Vol2-Iss2-Nanotech-Fig-1-300x169.jpg)
Figure 1: Comparison of nanoscale materials with common objects. [16] (Released)
It is unclear how devices and products composed of nanomaterials might affect human tissue once placed in the body. Forty-three nanopharmaceuticals are available in the global market, and countless other nano-products are being developed. [2] Although the European Commission recently issued guidance on the potential health effects of nanomaterials in medical devices, [3] the U.S. Food and Drug Administration, the U.S. government agency responsible for the approval and regulation of medical devices and pharmaceuticals, said in 2008 it did not see the need to have specific regulations for nano-engineered materials. [4] Last year, the FDA issued guidance on the use of nanotechnology in the products it regulates. While the FDA reiterated it has not developed a regulatory definition of nanotechnology, it did issue points for consideration; however, these were purely scientific in nature: [5]
1. Whether a material or end product is engineered to have at least one external dimension, or an internal or surface structure, in the nanoscale range (approximately one nm to 100 nm)
2. Whether a material or end product is engineered to exhibit properties or phenomena, including physical or chemical properties or biological effects that are attributable to its dimension(s), even if these dimensions fall outside the nanoscale range, up to one micrometer (1,000 nm)
Nanomaterials have become ubiquitous in society, and their use will rapidly increase. The United States is one of the leaders in nanotechnology research. However, the general lack of knowledge most patients have regarding nanotechnology is a prime issue. An even greater issue and challenge is how to understand, explain, respect and manage personal belief systems and normative values in regards to medical treatment pertaining to nanotechnology. Nanotechnology is a difficult concept to explain to the average person, and the United States is a pluralistic society in terms of its cultural makeup. This makeup will make addressing nanotechnology, while also being mindful of language barriers and cultural and religious values, in medical care difficult.
Culture is the shared language, beliefs, values, norms, behaviors and material objects that are passed from one generation to the next. Race is a group of people with inherited physical characteristics distinguishing them from another group, and ethnicity refers to people who identify with one another on the basis of common ancestry and cultural heritage. Although they are often used interchangeably, race and ethnicity are different; this is a critical point to remember. A fundamentally important part of most societies is religion, and this is especially true in the United States where more than 80 percent of the population has some sort of religious affiliation. [Table1]
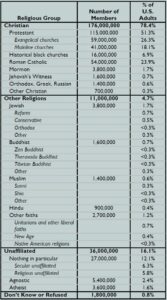
Tavle 1: How U.S. adults identify with religion. [8] (Released)
comprise nearly 78 percent of the population, [7] and they have historically been the dominant racial group. However, men still hold a significant amount of power and influence even though the gender distribution is roughly equal. In regard to religion, more than 78 percent of the population identifies as Christian, and the clear majority, 51 percent, are Protestant. [8] Except for gender, power is equivalent to numerical superiority in the United States, which is rare in the world. This is reflective of a representative democracy, and a good reason why de Tocqueville and others warned against the tyranny of the majority.
Very little has been published specifically addressing how religions and certain ethnic groups perceive the use of nanotechnology in medical applications. A few studies have addressed general perceptions of nanotechnology and stratified those results by various categories including religion, race and ethnicity. However, very little writing has been specifically aimed at addressing minority views. The majority of the literature either generally addresses religious and ethical views of nanotechnology (or technology in general) or overall cultural competence in the practice of medicine. As nanotechnology is used more frequently in medicine, there will be a need to integrate the concept into cultural training and practice. In 2006, the Commission of the Catholic Bishops’ Conference of the European Community released a statement on nanomedicine. The statement presented a fairly scientifically accurate account of nanomedicine and also raised concerns regarding how the use of nanotechnology could lead to abortion or euthanasia. Catholic Doctrine upholds the sanctity of life at all costs, and this is a concern that will most likely need to be addressed considering more than one billion people (16 percent) world-wide practice Catholicism, including 24 percent of the U.S. population. [9] In addition to the specific medical concerns raised by the Catholic Bishops’ commission, two other key issues regarding the use of nanotechnology in medicine have raised concerns among religious leaders. The issue of human enhancement is concerning because the development of devices and regenerative techniques could unnaturally produce human beings that are smarter, faster and stronger than the current species. Images of the Six Million Dollar Man, the Bionic Woman and RoboCop come to mind. In particular, this undermines the Christian notion of embodiment, in which human beings are to be comfortable with their imperfect bodies.
In addition, a more philosophical issue lies with the possibility that nanotechnology in medical applications could somehow reengineer humanity and lead to transhumanism, using human technology to accelerate natural processes in evolution, undermining the notion of creation. This would certainly shake the very fabric of most religious beliefs.
Another issue is the potential for the creation of some sort of inhuman creature or monster. In traditional Jewish cautionary tales, this is known as a golem, a creature created for either a destructive or protective purpose, and complete control rests with the creator. In modern society, Frankenstein’s monster would be the equivalent. While this aspect of nanomedicine is more mythological and derived from a primal fear of the unknown, the notion must be considered at least for potential violations of ethical codes. Either way, human enhancement or abhorrent creation would clearly violate most religious codes, especially in Western monotheistic religious tradition, as it would put humanity in the creator seat.
Some other religious considerations involve the uniquely American religions: Latter Day Saint Movement, Seventh-day Adventist Church, Christian Science and Jehovah’s Witnesses. All of these religions believe in Western medical treatment but with restrictions. For example, Jehovah’s Witnesses refuse blood products. It is assumed this belief will also include any future nanomedical use involving blood or blood products. Rastafarians are adamantly opposed to consuming any unnatural products, and while certain nanoparticles, such as carbon nanotubes, are made of commonly occurring natural substances, it is unclear whether there would be prohibitions regarding the unnatural manipulation of natural substances.
Moving past religion, there is a paucity of research regarding ethnic and other cultural views and beliefs regarding nanotechnology, certainly in medical applications, for both minority groups and all peoples and traditions in general. Studies have provided some knowledge on which cultural groups are more aware of nanotechnology versus others, but very few studies have actually looked at specific viewpoints and needs. Considering the lack of available information in this area, most discussions center around what is currently known about typical patient reactions to medical practices based on culture and how those reactions might be aggravated by nanotechnology. Historically, African-Americans have been cautious regarding the use of new technologies in clinical settings, especially if the technology is not clearly explained. This is an unfortunate fallout from the “Tuskegee Study of Untreated Syphilis in the Negro Male,” a tragic experiment funded by the Public Health Service from 1932 to 1972 in which 399 African-American males with syphilis in the rural South were left untreated, even though here was a well known cure, and followed until their death to study the progression of the disease. [10] While skepticism may still be present, being transparent and clearly explaining the use of nanotechnology and its purpose will be crucial for this group.
Symbolism plays an integral role in the mythos of all cultures. The symbolic perception of engineered nanomaterials themselves raises interesting questions. For example, Korean culture prohibits the presence of white chrysanthemums in hospital rooms because they are only used for funerals. A common type of nanomaterial structure is a nanoflower. Nanoflowers are so named because they are chemical structures that microscopically resemble flowers. The similarity between chrysanthemums and certain nanoflowers is uncanny.

Figure 3: A white chrysanthemum (left) compared with a ZnO nanoflower developed by ultrasonication method (right). (Released)
Explaining the concept of a nanoflower to a Korean-American who might be uncomfortable with a funerary object being placed inside his body is truly a unique situation, and one that most, if not all, providers are unprepared to face. Often overlooked societies include institutions such as the military. Though made up of different multicultural groups, the military has its own distinct culture. A key issue with military medicine is the lack of autonomy that combatants have during the course of war. This is known as enforced treatment. There are certain conditions where enforced treatment is necessary but difficult to understand. During the Persian Gulf War, it was determined that the threat of an attack with a nerve agent was likely imminent, and commanders made the decision to administer pyridostigmine bromide for prophylaxis. [11]
Pyridostigmine bromide has side effects, and commanders denied the autonomous taking of it, knowing some soldiers would likely refuse treatment on their own. This is a common practice in the military. The argument is based on a patriarchal foundation that those in charge know best and will make decisions for the greater good, even if that undermines personal choice. Although providers may disagree, they often have less choice than their patients, which does not create an encouraging environment that embraces cultural awareness.
Perhaps one of the least understood uses of nanomedical technologies in military practice is for human performance modification. This would certainly have combat implications since the armed forces could potentially create a Captain America-type figure to fight battles. Many techniques exist that could improve warfighters. In 2012, Nokia filed a patent for a nano-enabled tattoo that would vibrate when a cell-phone is active. Although strange and unique, this could improve communications capabilities on the battlefield. Similar devices could be used on the battlefield as sensors to alert soldiers to the presence of chemical or biological agents. [12]
The use of nanotechnology in medical applications may create scenarios in which new ethical problems, or exaggerated concerns of old problems, must be evaluated with respect to ethical, legal and social aspects. [4] At times, traditional theories of bioethics neglect social and cultural factors. [13] In order to accommodate the introduction of nanotechnology in traditional medical models, the concept must be introduced into the healthcare lexicon. This can be done by infusing the concept of nanotechnology into models of cultural competence. A well-known model of cultural competence in healthcare was developed. This model postulated that becoming culturally competent was a developmental process, and a culturally competent system would consist of five elements: [14]
1. Value diversity;
2. The capacity for cultural self-assessment;
3. Being conscious of the dynamics inherent when cultures interact;
4. Institutionalized cultural knowledge; and
5. Developed adaptations to diversity.
Furthermore, attitudes, policies and practices must be congruent within all levels of the system. This can be achieved by developing and implementing specific plans to incorporate the topic of nanotechnology into current culturally competent practices. Additionally, infusing the issues and basic concepts of nanomedicine into curricula approved by associations responsible for credentialing provider education, such as the Association of American Medical Colleges, would inform future providers entering into practice.
![Figure 4: Potential for a spiral of impaired trust in military medicine. (Released) [17]](https://hdiac.org/wp-content/uploads/2015/07/201506-Vol2-Iss2-Nanotech-Fig-4-300x281.jpg)
Figure 4: Potential for a spiral of impaired trust in military medicine. (Released) [17]
About the Author:
Greg Nichols is the program manager for the Nanotechnology Studies Program at ORAU in Oak Ridge, Tenn., where he provides expertise on nanotechnology-related topics. Previously, he supported a variety of occupational and environmental health projects for corporate and government clients. Nichols spent 10 years in various healthcare roles. He has published on a variety of topics in peer-reviewed journals and co-authored a book chapter on the use of epidemiology in risk assessment. He has a bachelor’s degree in philosophy and a Master of Public Health degree, both from the University of Tennessee and holds the Certified in Public Health credential.
References:
[1] Feynman, R. (1959, December 29). There’s Plenty of Room at the Bottom.
[2] Weissig V., Pettinger, T., & Murdock, N. (2014). Nanopharmaceuticals (part 1): Products on the Market, International Journal of Nanomedicine, 9, 4357-4373.
[3] Scientific Committee on Emerging and Newly Identified Health Risks (SCENIHR). (2015). Guidance on the Determination of Potential Health Effects of Nanomaterials Used in Medical Devices. European Commission.
[4] Boisseau, P. and Loubaton, B. Nanomedicine, Nanotechnology in Medicine. (2011). Comptes Rendus Physique,12, pp. 620-636.
[5] Food and Drug Administration. (2014). Guidance for Industry Considering Whether an FDA-Regulated Product Involves the Application of Nanotechnology.
[6] Durkheim, E. (1912). The Elementary Forms of Religious Life. In Sociological Theory in the Classical Era: Text and Readings. Sage
Publications, Inc. 2005.
[7] United States Census Bureau, State and County QuickFacts, 2014.
[8] Pew Research Religion and Public Life Project, Religious Landscape Survey.
[9] Pew Research Center, The Global Catholic Population.
[10] Centers for Disease Control and Prevention, U.S. Public Health Service Syphilis Study at Tuskegee.
[11] Beam T. (2003). Medical Ethics on the Battlefield: The Crucible of Military Medical Ethics. In Military Medical Ethics: Volume 2.
[12] National Academy of Sciences. (2012). Human Performance Modification: Review of Worldwide Research with a View to the
Future.
[13] Hedgecoe, A. (2004). Critical Bioethics: Beyond the Social Science Critique of Applied Ethics. Bioethics. 18 (2) pp. 120-143.
[14] Cross, T., Bazron, B., Dennis, W., & Isaacs, M. (1989). Towards a Culturally Competent System of Care: A Monograph on Effective Services for Minority Children Who are Severely Emotionally Disturbed.
[15] Rogers Commission, 1986. Report of the Presidential Commission on the Space Shuttle Challenger Report.
[16] Yokel, R., and MacPhail, R. (2011). Engineered Nanomaterials: Exposures, Hazards, and Risk Prevention. Journal of Occupational
Medicine and Toxicology. 6 (7).
[17] National Academy of Sciences. (2008). Military Medical Ethics: Issues Regarding Dual Loyalties: Workshop Summary.


